Silicone- Polydimethylsiloxane (PDMS)
Silicone (silastic) is one of the most maligned and hence, most studied biomaterial used in medicine today. It’s a synthetic non-resorbable polymer consisting of repeating ‘Siloxane’ monomers (Silicon, oxygen, and a saturated hydrocarbon side group). Poly-dimethyl siloxane [-(CH3)2Si-O-]n where methyl forms the side chain is used in most medical applications.
Depending on the length (n) and degree of cross-linking of the PDMA chains, the mechanical properties of silicone can change to fluid (short, straight chains- <30 monomers), gel (lightly cross-linked chains), or rubber (greater degree of cross-linking– > 3000 monomers).
Advantages of Silicone
- Highly biocompatible- inert, nontoxic, nonallergic
- Resistant to resorption
- Easily to sterilize
- Safe- has no proven association with systemic diseases like autoimmune connective tissue disease, neurologic disease or breast cancer. [Anaplastic large cell lymphoma (ALCL) associated with textured silicone breast implants is extremely rare, is a lymphoma, not carcinoma]
Disadvantages of Silicone
- Nonporous- hence, not incorporated–> hard fibrous encapsulation– sometimes painful and disfiguring.
- Smoothness- prone to extrusion, displacement– leads to removal.
- Silicone rubber has low tensile strength and may tear easily- eg. in finger joint implants. 💡
- The silicone gel in silicone rubber shell can diffuse out (gel bleed- thus altering its physical property), or rupture out- implant failure– which may be difficult to remove from soft tissue (inflammatory reaction- not proven). Hence the shell is made of fully polymerized
silicone with an amorphous (noncrystalline) silica filler added for strength. - Fluid silicone (low molecular weight) as injectable soft-tissue filler led to severe tissue
reaction and migration of the silicone and hence not used. - Implants and expanders are Expensive.
Uses of Silicone
1. Tissue expansion
2. Breast augmentation
Most breast implants are Silicon gel encased in a ‘silicone elastomer shell’ – they can be classified based on:
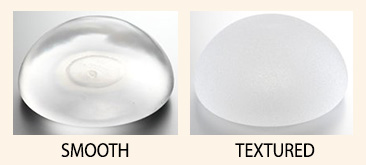
a. Surface– Smooth or Textured (less capsule formation, less mobile).
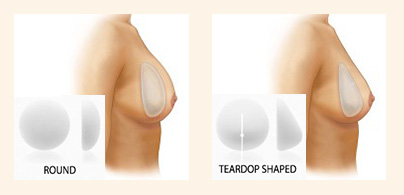
b. Shape– Round or Teardrop (more natural shape).
c. Projection/Profile– low, moderate, moderate plus, high, ultra-high.
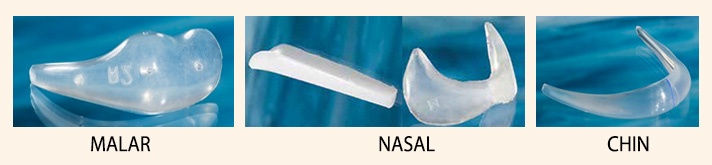
3. Chin, nasal, malar augmentation
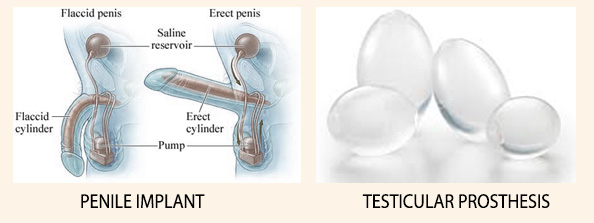
4. Penile and Testicular implants
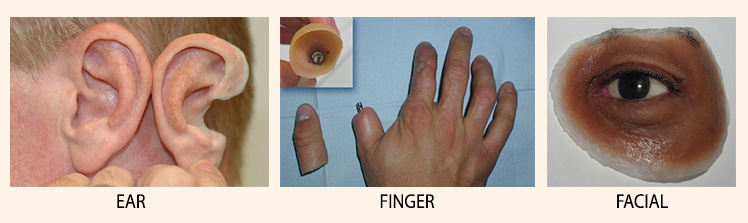
5. Ear, Finger, other Facial Prostheses
These prostheses can be either osseointegrated or tightly fitting which are custom-made, shaped and colored to match the anatomy of the structure it’s replacing, as closely as possible. They mainly supplement aesthetically, but can also have a minimal function.
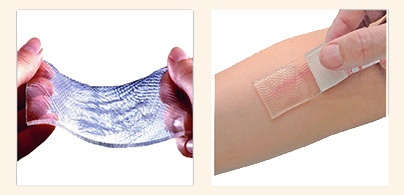
6. Hypertrophic scar or keloid treatment
Silicone Gel Sheets (SGS) and gel are used for the above. The mechanism by which it works is described in subsequent post.
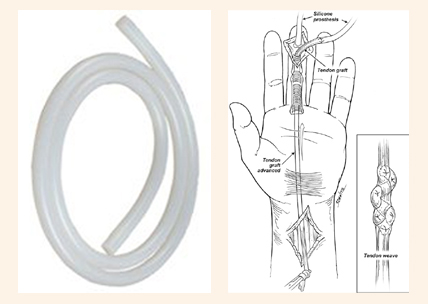
7. Hand surgery
- Small joint arthroplasty
- Delayed Flexor tendon replacement- 2 staged (Hunter’s tendon rod)
- Bone block spacers
If you found this post useful subscribe below for more such articles & subscribe to our YouTube channel for video tutorials. You can also find us on Facebook, Twitter and Instagram.
Bibliography
- Neligan’s Plastic Surgery- Vol 1- Principles- 4Ed (2017)
- Textbook of Plastic, Recon, Aesthetic Surgery- Vol 1- Principles and Advances in Plastic Surgery- Agrawal, Bhattacharya- 1Ed (2017)

Tutorials & tips in Plastic Surgery
+ Weekly updates of high-quality webinars!