Radford C Tanzer in 1959 first described the total reconstruction of the external ear with autologous costal cartilages (ACC) and thus began the new era of auricular reconstruction. Since then, several modifications and advancements have been made to the technique, mainly by:
- Burt Brent (USA)- 1974
- Satoru Nagata (Japan)- 1993
- Françoise Firmin (France)- 2010
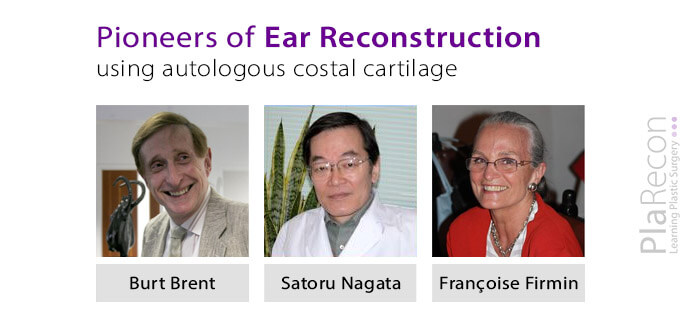
The differences between the techniques of autologous/ autogenous ear reconstruction for microtia as described by Dr Brent, Dr Nagata and Dr Firmin along with the advantages and disadvantages of each have been discussed below.
Comparison of Brent, Nagata & Firmin techniques
| Brent | Nagata | Firmin | |
|---|---|---|---|
| Age of initiation of 1st Stage | 6 years | 10 years & after the chest circumference at the level of the xyphoid ≥ 60 cm | 10 years |
| Number of Stages | 4 | 2 | 2 |
| Interval between stages | 3 months | 6 months | 6 months |
| Surgery (Individual) time | Short | Long | Long |
| Cartilage harvest side | Contralateral | Ipsilateral | Ipsilateral |
| Cartilages for framework creation | 6+7 synchondrosis- Base + retro-auricular wedge (banked), 8 helical rim | 6+7 synchondrosis (Base + Tragal extension), 8 (helical rim, crus helicis), 9 (antihelix, superior and inferior crus) +5 (in 2nd stage)- crescent-shape wedge for framework elevation | 6+7 synchondrosis (Base, Tragus-antitragus) 8 (Helix, Antihelix) +/- 9 (additional helical length) |
| Costal cartilage harvest | With perichondrium | Entire perichondrium left behind- The remnant cartilages are cut into 2 mm to 3 mm blocks and returned to the perichondral pockets (Kawanabe-Nagata modification- 2006) | Anterior perichondrium harvested with the cartilage, Posterior preserved. [Note: Synchondrosis used for the base is turned over, i.e. the perichondrium on the anterior surface becomes the posterior surface of the base while the posterior surface of the rib is carved and becomes the anterior surface of ear] |
| Framework integration | Few 4-0 Nylon sutures | Thin (38) gauge wires | 5-0 Steelex® (B Braun) stainless steel threads, double-armed with straight needles |
| Tragus creation | 4th Stage- Chondro-cutaneous graft from opposite ear concha. | 1st stage- Costal cartilage | 1st stage- Costal cartilage |
| Lobule creation | 2nd stage- Lobule transposition | 1st stage- W-incision & J-incision - Lobule split antero-posteriorly | 1st stage- Z-plasty incision |
| Lobule | Better | Compromised | Better |
| Framework elevation | Framework along with a layer of soft tissue elevated | Framework along with a layer of soft tissue elevated + | Elevation such that Cartilage base of the framework is exposed |
| Skin graft Type | Full Thickness Skin Graft (FTSG) | Ultra Thin Delicate- Split Thickness Skin Graft | Split Thickness Skin Graft (STSG) |
| Skin graft Donor site | Contralateral post-auricular | Ipsilateral occipital (over TP facia) | Ipsilateral occipital (over TP facia) |
| Ear projection | Lesser | Better | Better |
| Skin flaps secured over the 3D framework with | Suction drain | Bolster dressing- for two weeks post-op | 2 suction drains (15 Fr round blake) for 3-5 days post-op +/- Bolster dressing |
Advantages and Disadvantages
BRENT technique
Advantages
- Lower complication rates
- Shorter learning curve
- The framework has a lower profile- useful when the ear reconstruction site skin is tight.
Disadvantages
- Multiple surgeries needed for reconstruction (Four stages)
- The shape of the tragus is not perfect + the antitragus and inter-tragal notch are not prominent.
- The opposite ear is scarred for conchal composite graft for tragus reconstruction (Also- not available in B/L cases)
- Projection of the ear is lesser- the retro-auricular sulcus skin graft contracts over time
- Comparatively higher rate of framework resorption- esp. helix and antihelix- creating notches
- Higher risk of chest wall deformity and pneumothorax
NAGATA technique
Advantages
- Requires fewer stages
- Aesthetic improvements: every anatomic detail (including tragus and antitragus) of the reconstructed ear is prominent, projection of ear is better & symmetrical
- No chest wall deformity
- Costal cartilage regenerated in the perichondral pockets can be used when required- secondary auricular reconstruction/ bilateral cases
- Maximal preservation of blood supply(with preservation of pedicle in the conchal region- something Firmin didn’t believe in) with minimal risk of resorption of the grafted cartilage
Disadvantages
- Longer learning curve
- Good surgical and artistic finesse required, or else- higher complication rate and unsatisfactory outcome
- Risk of necrosis of lobule that is transposed in the 1st stage and other skin flaps (esp. the posterior flap- as its thinner and more extensively raised, the framework has a higher profile and bolster SS wire sutures are used)
- Costal cartilage is harvested in 2nd stage too (twice)
- Risk of wire extrusion– may lead to infection (can be prevented by embedding the wires properly)
- The use of temporoparietal fascia flap limits its use in future reconstruction + associated with the complication of alopecia
FIRMIN technique
Advantages
- Its unifying surgical classification schema helps manage any type of microtia based on the requirement. With the combination of the algorithm below- a complete operative plan for both stages can be created at the beginning:
- Framework: Type I, II, or III – with projection: PI, PII, or PIII
- Skin approach: Type 1, 2, 3a, or 3b
- Second stage: Type A, B, C, or D
- Better vascularity of reconstructed lobule (with Z-plasty like incisions)
- Remnant framework cartilages are banked in subcutaneous tissue under thoracic skin, so rib harvest is not required in the 2nd stage.
- + other advantages- similar to Nagata’s technique.
Disadvantages
- Longer learning curve, need for artistic finesse and risk of wire extrusion- similar to Nagata’s technique.
REREFENCES (For further reading):
Index articles:
- Brent B. Ear reconstruction with an expansile framework of autogenous rib cartilage. Plast Reconstr Surg. 1974 Jun;53(6):619-28.
- Nagata S. A new method of total reconstruction of the auricle for microtia. Plast Reconstr Surg. 1993 Aug;92(2):187–201.
- Firmin F. State-of-the-art autogenous ear reconstruction in cases of microtia. Adv Otorhinolaryngol. 2010;68:25-52.
Other articles:
- Olshinka A, Louis M, Truong TA. Autologous Ear Reconstruction. Semin Plast Surg. 2017;31(3):146-151.
- Baluch N, Nagata S, Park C, et al. Auricular reconstruction for microtia: A review of available methods. Plast Surg (Oakv). 2014;22(1):39-43.
- Justicz N, Dusseldorp JR, Shaye D. Firmin technique for microtia reconstruction. Operative Techniques in Otolaryngology-Head and Neck Surgery. 2017;28(2):90-96.
- Firmin F, Marchac A. A novel algorithm for autologous ear reconstruction. Seminars in Plastic Surgery. 2011;25(04):257-264.
- Firmin F. Ear reconstruction in cases of typical microtia. Personal experience based on 352 microtic ear corrections. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery. 1998;32(1):35-47.
Acknowledgement: Part of the table of comparison was compiled by Dr Gaurav Shetty, Microsurgery Fellow, Tata Medical Center, Kolkata.

Tutorials & tips in Plastic Surgery
+ Weekly updates of high-quality webinars!




Very informative and easy to grasp.. Especially for us (beginner)
Glad the article was helpful.