We learnt about the various aspects of keloid and how they are different from hypertrophic scar. Here we will look into the various ways of managing them. Though there are lots of options, it’s a challenging condition to treat effectively and often a combination of various options are required (multimodal).
We know, keloid has a genetic and racial predisposition, but even in the predisposed- it may still be prevented by the following prophylactic measures:
- Minimising inflammation at the wound/ surgical site and achieving primary healing (7-14 days) by:
- incision along RSTL (Resting Skin Tension Lines) or creases
- gentle tissue handling
- adequate debridement to prevent infection
- careful suturing
- using thin sutures with low tissue reactivity (monofilament)
- non-strangulating suturing techniques
- early suture removal or subcuticular sutures
- reducing suture line tension (eg. with Z plasties)
- Early pressure therapy with/without silicone gel sheeting [Details below]
- Adhesive taping across the scar esp. over the joints.
While these preventive measures, that basically reduce scar formation, form the base (and should be monitored by regular 4-6 weekly follow-ups till the scar matures), the treatment strategy should be initiated as soon as the symptoms and signs of keloid (raised, hyperpigmented, dried, painful, and itchy scars in high-risk areas) become apparent.
However, more often, we would get to see keloids for the first time at a later stage (matured).
The various treatment options (arranged in the order of clinical use) are as below:
Intralesional steroid injection
Intralesional corticosteroid injection is usually the first line of treatment for keloids.
Triamcinolone acetonide (TAC, Kenalog): 10-40 mg/ml every 4-6 weeks till the desired effect is achieved (usually, for 6 months or more).
Technical tips:
- As a large amount of pressure is required to inject the steroid into the toughened keloid (needle displacement, splashing and wastage), a Luer-Lock syringe is desirable but a cheaper and easily available option is a disposable insulin syringe with a pre-fixed needle.
- While local anaesthesia/block may be given separately, do not mix steroid in the syringe with Lignocaine +/- epinephrine (thought to reduce the sting/pain of injection under pressure) as lidocaine with epinephrine creates an acidic environment acidic (pH 4.7) and causes a burning sensation during infiltration- thus adding to the pain.

Effectiveness:
- Response is seen in 50-100% but recurrence in 9-50%
- Reduces symptoms: pain and itchiness
- Is a good peri-operative adjunct to intra-lesional excision to prevent recurrence or can also be used with cryotherapy.
Mechanisms of action– not fully understood, but are possibly:
- suppression of the inflammatory process (main)
- reduction in collagen and glycosaminoglycan synthesis
- inhibition of fibroblast growth
- enhanced collagen and fibroblast degeneration
Side effects:
- Subcutaneous/dermal atrophy
- Telangiectasia
- Pain at the injection site
Surgical excision of Keloid
Surgical excision should be tried after the scar/keloid matures (i.e. doesn’t blanch) and stabilizes (doesn’t proliferate) and it may take 8 months to about 2 years after the initial injury/insult.
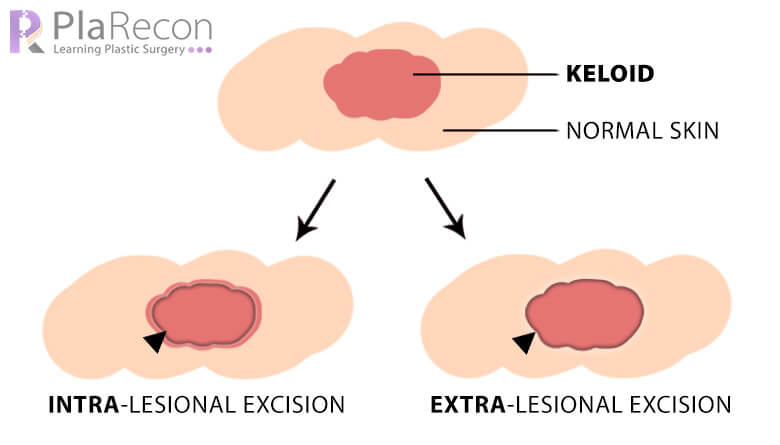
The surgical options are:
- Intralesional excision
- Extralesional or complete excision
1. Intralesional excision
It is the partial excision of the central portion of the keloid, leaving behind a thin peripheral rim of the keloid. Also, the excision does not extend beyond the deepest level of the dermis thus not exposing the subcutaneous fat.
It is used for keloids with a broad base (since primary closure can’t be achieved without tension) or for keloids in nonexpendable areas– Eg. on the pinna.
Further reading: Intralesional excision as a surgical strategy to manage keloid scars: what’s the evidence? → link.
2. Extralesional or complete excision
Complete excision is useful for small keloids or those with narrow-base, where tension-free primary closure can be achieved with minimal undermining after excision. [Slowly, it’s becoming the more favoured excision technique with more effective adjunct therapies reducing the recurrence rate after complete excision and with more efficient tension-free reconstructive options- like local perforator-based flaps]
Sometimes, very large and symptomatic (painful, itchy) keloids may necessitate extra-excision and cover with graft or flap (with or without pre-expansion) with all preventive measure as mentioned above to prevent keloid formation in their margins. Staged serial excision (with or without pre-expansion) can also be done.
Since recurrence rate after surgical excision of keloids is very high (>50%), surgical excision is often combined with other modalities like intra-lesional steroid, pressure therapy, silicone gel sheet, radiation and 5FU.
Pressure therapy
For keloids, pressure therapy is effective as a preventive modality or a post excisional adjunct to prevent recurrence rather than a primary treatment modality.
Most effective in ear lobe keloids post-resolution by intralesional steroid or intralesional excision where customised clip-on or magnetic earrings can be used.
Effective pressure: 24 to 30 mm Hg continuously for a minimum of 23 hours a day for 6 months, and it can be used for up to 2 years.
Possible mechanisms of action that may act to stabilize the keloid scar and prevent recurrence are:
- Reduces blood inflow → reduces the levels of soluble factors that promote inflammation and keloid formation.
- Activates cellular mechanoreceptors linked to the ECM → (+) fibroblast apoptosis, (-) myofibroblasts, ??(+) MMP-9 → ECM remodelling, reduced scar mass.
- Activates sensory nerve → translates the pressure into intracellular biochemical signal and gene expression → regulates the release of various cytokines that control the scarring process.
- Eases pain, itchiness; decreases edema → may help scar maturation.
Problems:
- Non-compliance, esp. in hot and humid summers → maceration (sweat), persistent pruritus, skin breakdown, rash and foul smell (sweat, any discharge)
- Inability to adequately fit the pressure garment (since with use, the elasticity of the garment decreased as the material wears off and the pressure also reduces as the height of the scar becomes smaller)
Pressure therapy is usually combined with Silicone gel sheeting to increase effectiveness.
Silicone gel therapy
Silicone gel sheeting (SGS) or gel application (esp. over mobile parts where sheeting won’t conform) are often used prophylactically or as a post-treatment adjunct along with pressure therapy. They are very useful in children in whom invasive therapies cannot be used.
Effective when used 12–24 hours/day for 3-6 months.
Possible mechanisms of action:
- Wound hydration by decreasing the transepidermal water loss to nearly half that of normal skin, causing a buildup of moisture on the skin surface under the silicone sheet → likely responsible for the decreased capillary activity, reduced hyperemia, and reduced collagen deposition. [Main mechanism rather than the effect of any inherent property of silicone.]
- Altered hydration → thought to cause electrostatic changes that influence collagen deposition and remodelling within the scar.
- Static electricity generated by friction → proposed as a plausible reason for silicone’s anti-scarring effect.
Emerging treatment options
- Intralesional 5-Fluorouracil (5-FU)
- Intralesional cryotherapy
- Radiotherapy (Brachytherapy)
- Lasers
- Topical Imiquimod cream
- Intralesional Bleomycin
- Intralesional Interferon (IFN)
- Botulinum toxin A (BTA)
- Topical Photodynamic therapy (PDT)
Some of the above are very new and innovative while some are being used in treatment of keloid for a couple of decades with mixed results, recent studies with revised doses and various combinations of modalities have rekindled interest. We will discuss more about them in a subsequent post.
Stay tuned and keep in touch by subscribing. Do let us know your views in the comments section below.

Tutorials & tips in Plastic Surgery
+ Weekly updates of high-quality webinars!




Thank you for explaining that surgical excision should take place after the scar matures which could take anywhere from eight months to two years. My sister has some keloid scars and she’s been wondering how to make it go away since it’s on her wrist and can make things really difficult to do. I’ll be sure to mention this to her and see if she’d be interested to talk to her doctor about this as a possible option.
Welcome. Yes, you may ask her to visit a Plastic Surgeon nearby for diagnosis and management.